Department of Chemical Engineering receives $3.5 million award to study impact of adolescent exposure to opioids
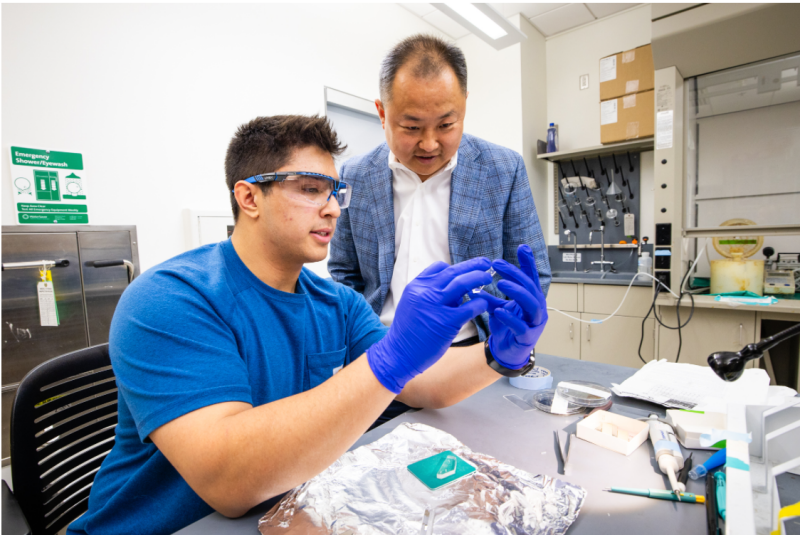
Chang Lu (right) and Ph.D. student Jacob Neide examine microfluidic device used in epigenomic assay
Opioid addiction is a pressing public health crisis with far-reaching implications. More than 100,000 deaths a year have been linked to drug overdoses since 2020.
The Centers for Disease Control and Prevention reports that more people died from drug overdoses in 2021 than from firearm and motor vehicle deaths combined. Three-quarters of these overdose deaths were attributable to opioids.
A five-year, $3.5 million grant from the National Institutes of Health’s National Institute on Drug Abuse will fund the Virginia Tech Department of Chemical Engineering’s pioneering research to understand how adolescent exposure may contribute to opioid addiction. Examples of adolescent exposure include youth taking prescribed opioid medication for pain relief following a sports injury or experiencing neglect in instances of parental opioid addiction.
Chang Lu, the Fred W. Bull Professor of Chemical Engineering and graduate chair, will serve as the contact principal investigator of the initiative, leading a team in the research.
Chemical engineers bring in unique skills
According to Lu, chemical engineers have a unique set of skills that they can leverage in chemistry, biotechnology, and process engineering to clarify how addiction takes hold, making it possible to eventually develop processes and products that alleviate the societal burden of drug addiction. Additionally, their proficiency in data analysis and modeling allows them to develop the tools required to unveil complex neural networks, opening new avenues for brain research.
Lu’s team in the initiative includes Julie Blendy, professor of pharmacology at the University of Pennsylvania, and Wei Wang, professor of chemistry and biochemistry at the University of California, San Diego.
Blendy’s expertise in long-lasting effects of adolescent oxycodone exposure on reward-related behavior and gene expression in mice make her an ideal collaborator for the initiative. Likewise, Wang brings proficiency in analyzing large data sets like the ones that will be generated in the research.
“My research at University of Pennsylvania focuses on understanding the molecular basis for the biochemical and behavioral changes that come with chronic drug use," noted Blendy. “How drugs lead to long-term adaptations within the brain to impact drug-taking behavior is not known, but alterations in gene expressions are likely involved. Our team — led by Lu — is well-poised to significantly advance the field in understanding the biological basis of addiction.”
A complex problem
Opioid addiction is a multifaceted issue, involving both genetic and environmental components. Genetic factors can predispose individuals to addiction vulnerability, influencing how their brains respond to opioids.
Environmental factors such as early-life adversity, social networks, and access to opioids play pivotal roles in addiction initiation and maintenance. Understanding how genes and the environment interact at the molecular level is central to understanding the neurobiology of addiction. Epigenetics, the study of how behaviors and environment can cause changes in how genes work, provides valuable insights into the gene-environment interactions that drive addiction.
In this project, Lu’s team will focus particularly on one environmental factor: How early exposure to opioids potentially contributes to addiction. "When adolescents are injured during sports, they are often prescribed strong pain relievers that contain opioids,” Lu said. “It is important to understand what footprint such early exposure leaves in a developing brain, in terms of epigenetic alterations.”
A bridge between genes and the environment
Epigenetics refers to hereditary changes in gene expression that do not involve alterations to the DNA sequence. Epigenetic modifications alter the accessibility of DNA and play critical roles in regulating gene expression and shaping an individual's response to environmental stimuli.
Many of the genes that are thought to play a role in opioid addiction are involved in the endogenous opioid system, which is the body's internal system for regulating pain, reward, and addictive behaviors. It consists of opioid substances produced naturally within the body, called endogenous opioids, and their receptors, into which opioids fit like keys into locks.
Opioids introduced from outside the body, called exogenous opioids, including opioid medications and heroin, also act on these receptors. Variations in the genes that provide instructions for making opioid receptors have been studied extensively as genetic risk factors for opioid addiction. Researchers hypothesize that differences in the receptors' structure and function influence how the body responds to opioids.
Using low-input epigenetic profiling techniques developed in Lu’s lab, the team is better able to study gene-environment interactions in the brain. These techniques will allow them to examine epigenetic changes within limited quantities of brain tissue, making it feasible to explore the dynamics of specific brain regions and cell types involved in addiction.
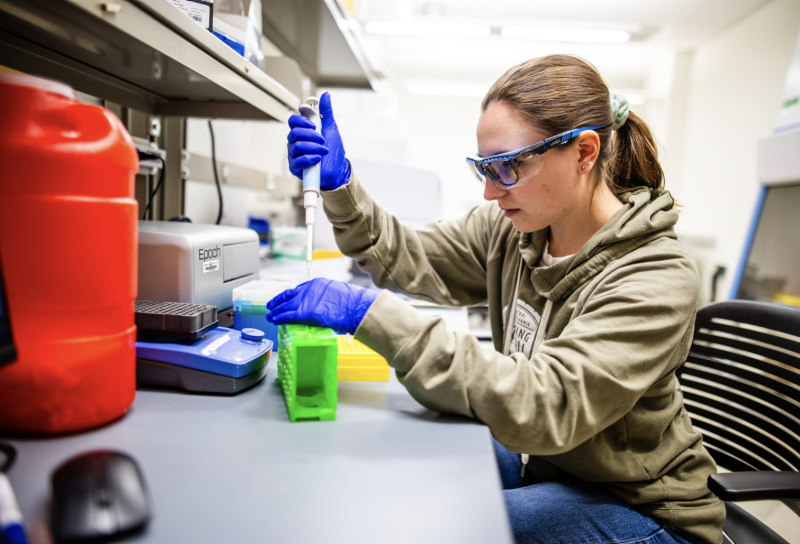
Jenna Catalano prepares epigenomic assays; photo by Peter Means for Virginia Tech
Key insights gleaned by this approach include
- Identifying epigenetic biomarkers. These biomarkers may serve as diagnostic tools for assessing an individual's risk of addiction or as targets for therapeutic interventions.
- Unraveling developmental trajectories. Epigenetic profiling can reveal how adolescent experiences and environmental factors shape epigenetic patterns over time, offering insights into critical windows of vulnerability to opioid addiction.
- Personalized medicine. Tailoring interventions based on an individual's epigenetic makeup may enhance treatment efficacy and reduce the risk of relapse.
- Informing policy changes. A fundamental understanding of how opioid addiction works in the brain can inform policy and regulatory decisions.
“Opioid addiction is a complex and devastating public health crisis,” said Lu. “Low-input epigenetic profiling is a powerful tool in unraveling the intricate gene-environment interactions that underlie addiction vulnerability and progression. By studying epigenetic dynamics within specific brain regions and cell types, we hope to identify biomarkers and shed light on when people – especially adolescents – are vulnerable to addiction, and why. Successfully doing so means opening the door to personalized treatment approaches and prevention strategies in the future.”



.jpg.transform/m-medium/image.jpg)
